The New York Times has just published an article supposedly examining the pros and cons of the elderly taking statins. On the face of it the article appears to be balanced however, there are a great number of errors and omissions in this article and as a result the article creates completely the wrong impression about statins.
The New Times Article can be found here, it might be worth comparing the article with the information below.
The first problem with the New York Times article is found in the second paragraph where the author incorrectly states “[statins] get much of the credit for the nation’s plummeting rates of heart attacks and strokes”.
In fact, heart disease death rates have been declining rapidly in the United States (and the UK) since the 1970s (see figure 1). Statins were introduced in the mid to late 1990s - around 20-25 years after the sharp decline was already well under way.
FIGURE 1
The reduction in heart disease deaths in the United States (and the UK) is mostly due to the reduction in the number of people who smoke cigarettes (see figure 2). Improvements in hospital treatments has also contributed.
FIGURE 2
In addition, retrospective studies have also failed to find any benefit associated with statins. Although statin clinical trials have predicted a slight reduction in heart attacks in some patient groups, studies that have looked retrospectively have found that these predicted benefits have not actually materialized.
Clinical trials are perceived as the gold standard of clinical research but in recent decades there has been a greater understanding of how the clinical trial process can be manipulated by commercial interests in order to get the result that is favorable to the company sponsoring the trial. Therefore, it is also important to look retrospectively at the risks and benefits as the drug is used widely in the general population.
For example, researchers collected data from all but one of the municipalities of Sweden and they found that statins had not provided any benefit despite a huge increase in usage.
In 2012 the British Heart Foundation published a report detailing a wide range of heart disease statistics. One of the highlights of this report was the decline in heart disease death rates that had been seen in the UK between the years 2002 and 2010. The report listed the improvements that had led to this decline in deaths - statins were not mentioned at all.
Doctors in the pockets of drugs companies and lazy reporters often repeat the myth that statins have contributed to the decline in heart disease deaths, but there is not any to data to support this.
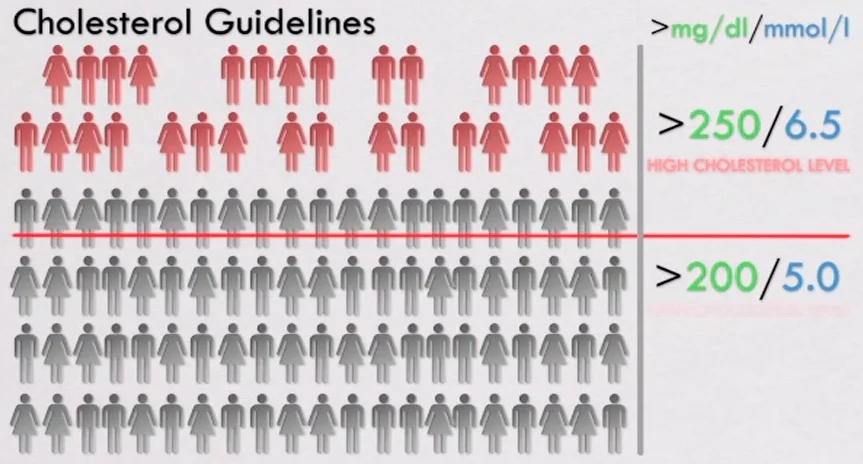
There are many other problems with the New York Times article, such as quoting relative percentages instead of absolute percentages (relative percentages hugely misrepresent the data), and also a failure to mention the other common adverse effects of statins that the elderly are more vulnerable to. However, I want to take particular issue with the fact that the New York Times article also fails to inform people of the strong connection between low cholesterol levels and shorter life expectancy and increased cancer rates - a correlation particularly strong in the elderly. As explained in the excerpt below from Statin Nation II:
References:
Figure 1 taken from Factors Influencing the Decline in Stroke Mortality
A Statement From the American Heart Association/American Stroke Association
https://doi.org/10.1161/01.str.0000437068.30550.cf
Available here
Figure 2 is published by the CDC and is available here
Swedish Study: Nilsson et al. No connection between the level of exposition to statins in the population and the incidence/ mortality of acute myocardial infarction: An ecological study based on Sweden's municipalities. Journal of Negative Results in BioMedicine 2011, 10:6
British Heart Foundation report: Coronary Heart Disease Statistics 2012. Available from https://www.bhf.org.uk/publications/statistics/coronary-heart-disease-statistics-2012








![Drawn using data from reference [2]. Showing the relationship between the number of 8oz (250ml) glasses of water consumed per day compared with the risk of dying of heart disease. Graph shown includes the data for Men.](https://images.squarespace-cdn.com/content/v1/5264f4ade4b01acd1ac81719/1468996773631-CX9H4HP2GHU9FXG8PPY3/image-asset.jpeg)